News and views
Read our latest news and updates.
For media inquiries, contact us at media@compasspathways.com
-
March 28, 2024
Compass Pathways Board Chair and Co-Founder George Goldsmith and Co-Founder Ekaterina Malievskaia St...
Read article
-
March 18, 2024
Recognising and celebrating neurodiversity
Read article
-
February 29, 2024
Compass Pathways Announces Fourth Quarter 2023 Financial Results and Business Highlights
Read article
-
February 28, 2024
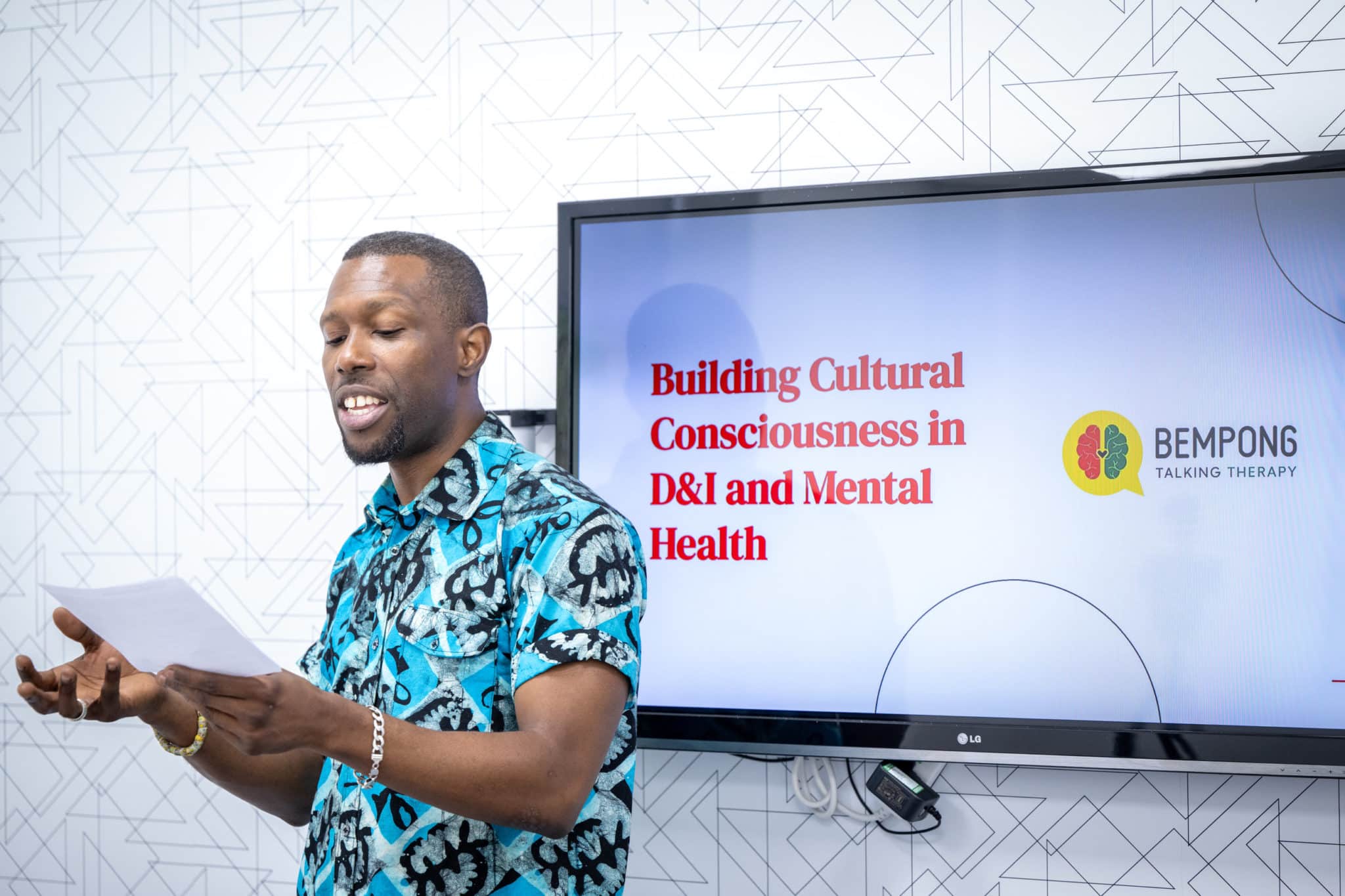
Exploring cultural consciousness with Jarell Bempong
Read article
-
January 16, 2024
Compass Pathways enters into research collaboration agreement with Hackensack Meridian Health to dev...
Read article
-
January 05, 2024
Compass Pathways and Greenbrook TMS enter into three-year research collaboration agreement
Read article
-
December 19, 2023
Compass Pathways announces investigational COMP360 psilocybin treatment was well-tolerated in phase ...
Read article
-
December 07, 2023
Compass Pathways appoints Teri Loxam as Chief Financial Officer
Read article
-
December 06, 2023
Study results of psilocybin treatment in bipolar II depression published in JAMA Psychiatry
Read article
-
November 15, 2023
Compass Pathways initiates UK component of global phase 3 study of psilocybin treatment in treatment...
Read article
-
November 02, 2023
COMPASS Pathways Announces Third Quarter 2023 Financial Results and Business Highlights
Read article
-
October 26, 2023
Compass Pathways announces CFO transition
Read article
Looking for older news and views posts? View Compass news archive