Our blog

For media inquiries, contact us at media@compasspathways.com
Looking for news? Read our investors news releases.
-
July 31, 2024
Compass’s hiking club
Read article
-
July 08, 2024
Joining a mission-driven team: talking to Lori Englebert, Compass’s new Chief Commercial Officer
Read article
-
May 20, 2024
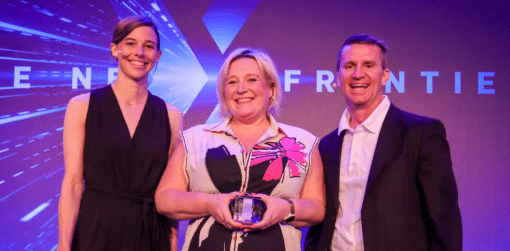
Recognising Quality at Compass
Read article
-
May 20, 2024
Celebrating Clinical Trials Day with Mike Gold, Compass’s new Chief Research & Development Of...
Read article
-
May 16, 2024
Advancing Digital Accessibility
Read article
-
May 14, 2024
Supporting our team’s wellbeing
Read article
-
March 18, 2024
Recognising and celebrating neurodiversity
Read article
-
February 28, 2024
Exploring cultural consciousness with Jarell Bempong
Read article
-
June 01, 2023
Celebrating Pride 2023
Read article
-
April 06, 2023
Talking to a Principal Investigator on our Phase 3 programme
Read article
-
March 08, 2023
Launching our Diversity Equity and Inclusion (DEI) council
Read article
-
February 16, 2023
Compass’s impact strategy
Read article